One month after opening up, the state of Arizona has become one of the country’s top COVID-19 hotspots.
Since May 26, the state has seen the now all-too-familiar continual upward trend in COVID-19 cases, hitting a single-day record in case growth on Friday at 1,654 new cases in one day and with a reported total caseload increase of 76 percent since May 28.
The unhindered growth in cases has sparked concerns that the state’s hospital capacity will be overwhelmed, with major hospital networks in the state publicly saying that they could see their ICU beds full in the span of a few weeks, if case growth continues unabated.
Since the state’s stay-at-home directive ended on May 15, Arizonans have largely lived without mandates to socially distance or wear masks when in public.
“When the stay at home order ended, the governor didn’t put any criteria for enforcement, compliance, or expectations on businesses that were enforceable whatsoever,” Will Humble, director of the Arizona Public Health Association and a former head of Arizona’s Department of Health Service, told TPM.
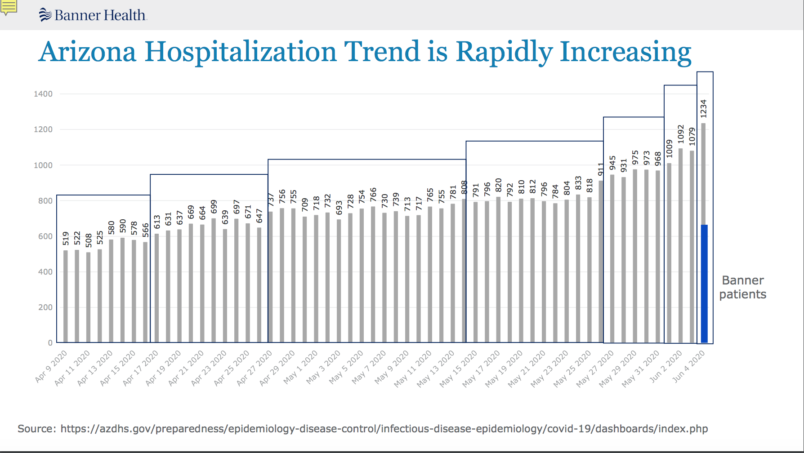
Banner Health, a hospital chain with a large Arizona presence, said last week that its hospitals were nearing capacity. Eighty-four percent of the state’s ICU beds were occupied this week; in Phoenix, it was higher, near 90 percent.
The company released a slideshow outlining the situation, including a graph of increased hospitalizations in the state — what epidemiologists look to as the true measure of the severity of an outbreak.
Humble told TPM that the current outbreak first began to show up in earnest between May 25 and 26 — ten days after the stay-at-home order came to an end.
He added that those 10 days “represent one incubation period plus testing delay after the end of the stay at home order — thats the inflection point.”
Humble went on to say that cases began to increase at an even higher rate in the week following Memorial Day, describing the holiday weekend as “throwing gas on the fire.”
Yet the state continues to lack both extensive testing and contact tracing, making it difficult to ascertain the true scale of the outbreak and contain it, according to Purnima Madhivanan, an associate professor at the University of Arizona’s college of public health.
“Those people that are exposed are going to continue to go on living their lives,” said Madhivanan. “You’re going to see they become infectious before they’re symptomatic — the shedding is already happening.”
Madhivanan described an environment with extremely limited signs that a pandemic was raging.
“It’s been appalling to see people acting like nothing has happened — sitting out in the coffee shops with no masks, just like pre-COVID,” she told TPM. “And we haven’t hit the peak — the major health systems are saying, get ready, have your plan B.”
“If the big health systems are saying that, then it’s happening,” she added. The remaining question is how far the outbreak will go in stressing the state’s hospital capacity.
State officials have taken what might be described as a hands-off approach towards the situation. State health director Cara Christ said at a Thursday press conference that “we are not going to be able to stop the spread but we can’t stop living as well.”
Governor Doug Ducey (R) has downplayed the idea that the state was nearing capacity in its hospitals, saying that “we are not in a crisis situation” and adding that field hospitals could pick up the burden.
To Humble, the question is less of ability to handle the oncoming waves of patients, and more is one of honesty.
“To look at hospital capacity dwindling, and to put your head in the sand and say, we’re going to rely on surge capacity, then you have an obligation to tell the people of Arizona that with that surge comes different standards of care,” Humble said. “You don’t get the same care in contingency or crisis mode — and that’s not just in field hospitals, that’s everywhere.”






