It took years. But doctors had nailed down, to the second, how to treat heart attack patients as quickly as possible.
Ambulance crews would radio ahead to the hospital that they were treating someone with a heart attack. The patient would never see the inside of an emergency room, and instead would be whisked away straight to a catheterization table, where doctors would decide whether to install a stent.
“Time is heart muscle,” Martha Gulati, chief of cardiology at the University of Arizona, told TPM.
Then COVID-19 hit.
Apart from the disease’s more well-known ravaging of the respiratory system, significant numbers of COVID-19 patients arrive at hospitals with serious heart problems, many of which first appear to be those of a heart attack but turn out to be symptoms of the coronavirus or the body’s response to it.
So doctors on the frontline of the COVID-19 pandemic have adapted, relying on new medical research from foreign hotspots like Wuhan and Lombardy to contend with how little we still know about the virus itself. Many hospital cardiology departments, for example, have begun to take potential heart attack patients with suspected COVID-19 into their ERs to first determine whether they have contracted the virus before moving “them back into the cardiac care path,” Thomas Maddox, chair of the American College of Cardiology’s Science and Quality Committee, told TPM.
He added that in hotspots like New York City, hospitals had “moved to a lower threshold: to test, and wait until it comes back, before doing anything with the patient.”
Maddox described the dilemma to TPM as a decision between bad variables. On the one hand, treating a COVID patient presenting heart symptoms as if he had a heart attack could expose the doctor. On the other, treating all patients as if they were infected with COVID could deprive those suffering from heart attacks of precious minutes.
“It’s been so hard to solve,” Maddox added. “Because, at the same time, you don’t want to take somebody who is short of breath because they’re having a heart attack and delay their treatment because you send them to a COVID unit, and miss the opportunity to help out their heart.”
The symptoms appear in different ways, experts told TPM. Some patients struggle with blood clots that course throughout their body, while others have severely inflamed hearts. Others still face organ failure amid spiraling blood oxygen levels.
“There’s not an easy way to tell, though, if they’re presenting so much like a heart attack,” Gulati told TPM. “We’re seeing reports of myocardial infarction when they have COVID-19, but often they aren’t always having blockages of the coronary arteries that we traditionally expect.”
She added that, in COVID-19 patients, lack of blood oxygen can creep up fast, overtaxing the heart.
“They are sitting there talking to you, and suddenly they go incredibly bad,” Gulati said, speaking of patients with dangerously low blood oxygen levels. “That is a big demand on the heart, if the heart is not getting enough oxygen, and the organs aren’t getting enough oxygen. As a result, everything is compromised.”
The lack of knowledge around COVID-19 and its symptoms can complicate diagnosis after death, as well.
Preliminary mortality data released by the Centers for Disease Control suggests that, as the pandemic peaked in New York City, the number of people dying due to what the CDC classifies as “diseases of the heart” also peaked.
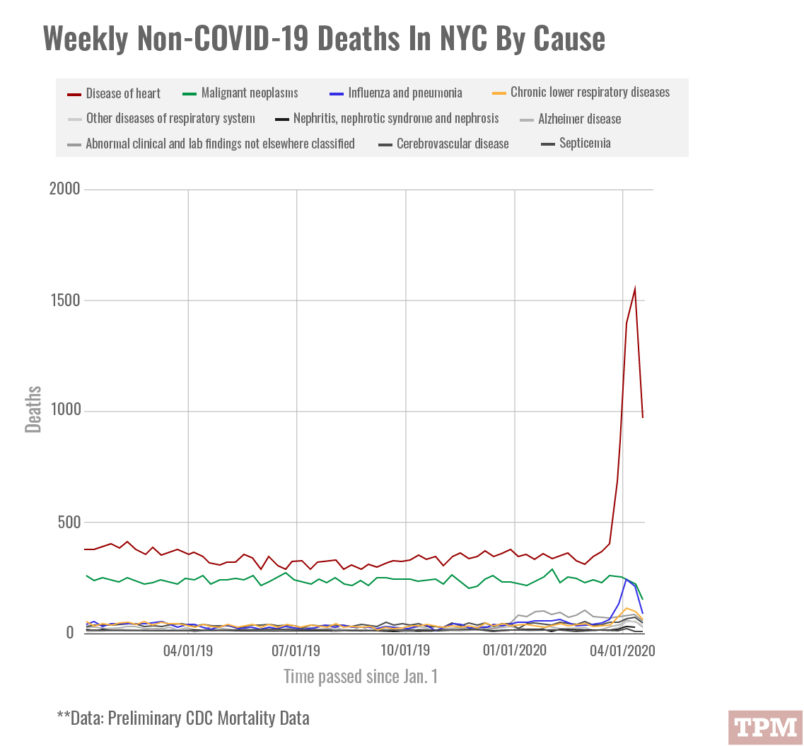
The data suggests that deaths related to heart problems went from an average of 350 per week to a peak of 1,558 in the week ending April 11.
Part of that may have to do with cause of death being difficult to determine in cases where hospitals are overtaxed, and medical examiners using sudden cardiac death to describe cases where the true cause of death was unknown.
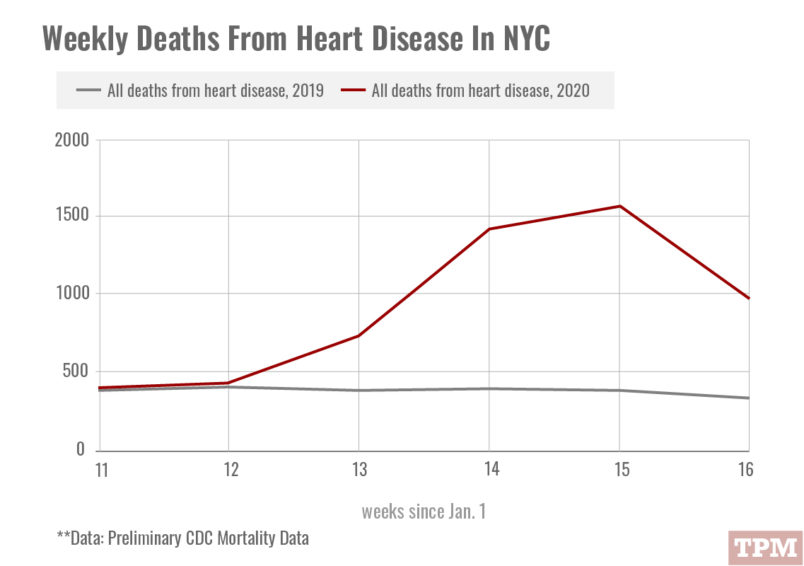
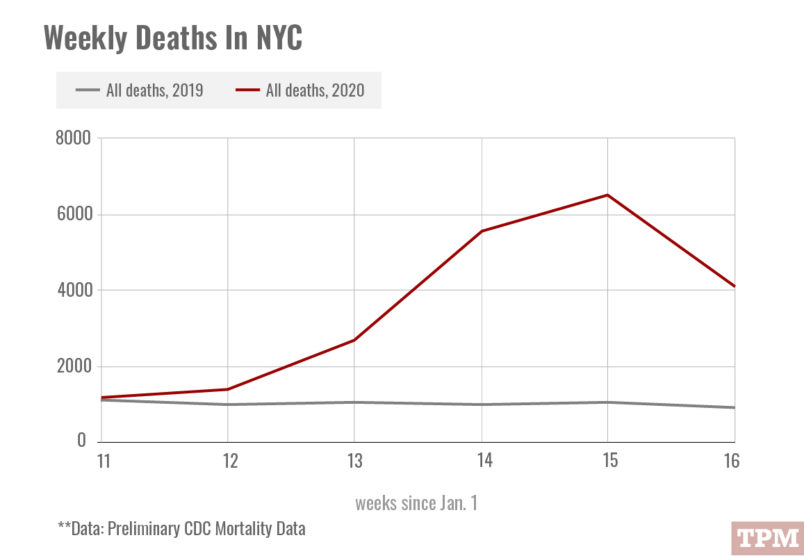
But it may also be a reflection of of what Sahil Parikh, a cardiologist at Columbia University Irving Medical Center in Manhattan, described to TPM as “direct and indirect effects of COVID-19” on the heart.
The heart symptoms of COVID-19 initially snuck up on doctors in Wuhan and Europe, who issued preliminary medical studies that were read widely in the U.S.
Parikh told TPM that the foreign medical reports gave the city’s hospitals and doctors an edge in treatment.
That lead, Parikh said, allowed hospitals to begin treating people presenting with heart attacks in March as actually suffering from COVID-19.
“It was relatively early along, and that’s due to us not being the first in the world to experience this disease,” Parikh told TPM. “So pretty rapidly as this was starting to rise in frequency, our teams locally and our national societies began to appreciate that we had to come up with a different strategy.”
Maddox, the American College of Cardiology committee chair, told TPM that his organization had arranged webinars with doctors in China and Italy
“We’ve been able to anticipate better,” Maddox said. “We’re more finely tuned in the complications that come with this and not be as flummoxed.”
He added that the webinars yielded useful, early information, including about cases where patients on ventilators faced serious heart issues after being taken off the devices.
“They weren’t having a traditional heart attack, you weren’t sure why it was happening,” Maddox said, adding that a conclusive explanation for the phenomenon remains elusive.
Parikh said that his hospital had temporarily ended processes designed to get heart attack patients onto a catheterization table as quickly as possible because “so many patients present with atypical symptoms.”
“They might look like they’re having a heart attack, and we might realize that its COVID-19 with heart attack manifestations,” he said. “So we could spare the patient an unnecessary procedure, and protect the patient and us from unnecessary exposure.”
Many people already afflicted with heart-related illnesses remain wary of coming into hospitals for regular treatment for fear of being infected with COVID-19. That may also partially account for the surge in heart-disease related deaths in New York. Others find themselves experiencing heart-related symptoms and fail to recognize it as COVID-19.
“People expected this to be like the flu,” Parikh said.
Charts compiled and designed by Jacob Harris and Christine Frapech.






