In the weeks since the unwieldy and politically unpopular task of dismantling the Affordable Care Act fell to the GOP Senate, Republican senators have been able to punt on some of the tough decisions in writing their repeal legislation until after they saw what the CBO said about the House Obamacare repeal bill.
That CBO report has now landed, and it doesn’t make GOP senators’ lives any easier. Wednesday’s report reinforced the many problems and ugly trade-offs in the House bill that Senate Republicans have been struggling with for months. It also dropped in their laps a new problem that was a result of an amendment added to the House bill that was scored for the first time in Wednesday’s CBO report: What to do about people with pre-existing conditions, whose protections under the ACA are significantly rolled back in a provision that allow states to opt out of Obamacare’s insurer mandates?
Here are five points on how the CBO score puts the big squeeze on Senate Republicans:
The waivers make pre-existing conditions protections very messy, if not impossible.
The big question for the CBO was the impact of a major, last-minute addition of a waiver provision to the House bill, which stands to violate GOP promises to protect those with pre-existing conditions.
The CBO found that one-sixth of Americans would live in states that would seek waivers so aggressive that it would create a wide variation in premiums for which the CBO did not even provide an estimate average. In those places, the individual market would grow increasingly unstable over time, as healthy people flocked to less generous plans that were allowed to medically underwrite based on health status. People with pre-existing conditions would in turn see premiums rise until some were priced out of coverage entirely. The extra $8 billion funding added to the House bill to subsidize them would not be “sufficient to substantially reduce” their “large increases” in premiums, the CBO said.
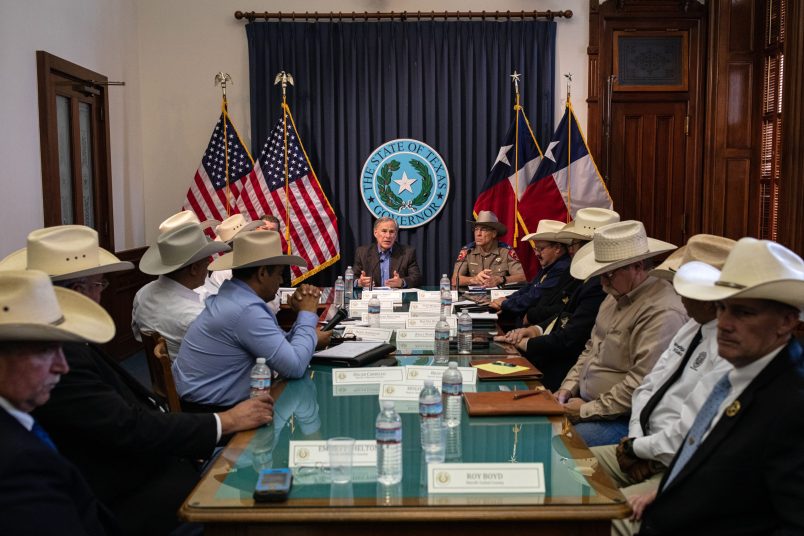
Senate Republicans have been generally open to a waiver idea, but many have insisted they want people with pre-existing conditions protected. So cleaning up that mess will be a top priority.
There’s no escaping 23 million people losing coverage.
The CBO’s top line coverage number was bad the first time the AHCA was scored and it hasn’t budged much since. Twenty-three million fewer Americans will have insurance by 2026 under the House-approved bill, which is hardly better than the 24 million in coverage losses predicted under the initial version. That downward tick in coverage losses comes in part, the CBO said, because the individual marketplace will be less attractive and more employers will thus continue to offer coverage than was projected in the March version of the legislation.
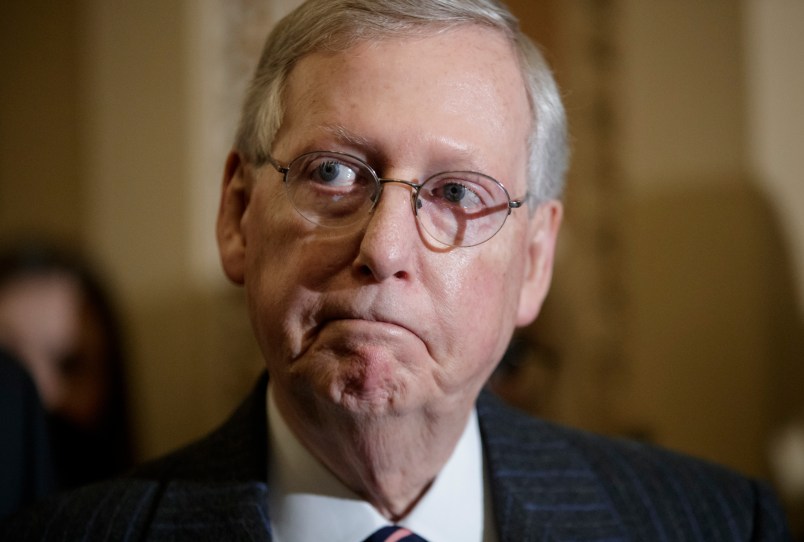
The first time around some Republicans cast doubt on the CBO’s predictive abilities and that strategy is already in play now. Nevertheless, some GOP senators have recognized those coverages numbers are far from ideal and floated more robust tax credits or a softer cushion to the Medicaid cuts as a way to improve them. The problem there, however, is that those tweaks will likely require more funding, and the Senate’s bill will still have to reduce the deficit by $119 billion over 10 years.
Medicaid remains the elephant in the room.
One of the biggest challenges in the Senate is an aspect of the House bill that hasn’t changed since the March CBO score: its massive cuts to Medicaid, which is at the heart of the legislation.
Of the 23 million fewer covered Americans under the GOP House plan, 14 million lose coverage due to the House bill’s phaseout of the Medicaid expansion and its overhaul of the larger program from an unlimited match rate to a capped system that limits funding on a per enrollee basis.
This gutting of Medicaid saves the government $834 billion, which in turn finances the $664 billion in tax cuts to industry and high earners under the House bill. But the Medicaid cuts also pits expansion state senators against non-expansion state senators. And the formula used to cap the traditional program hits different states in different ways, also complicating the bill’s path to 51 votes for Senate passage.
Older people and poor people lose out under the GOP’s tax credits.
Wednesday’s CBO report reinforced a point made in its analysis of the original version. AHCA’s tax credit scheme severely shortchanges lower income consumers and older people, the latter a key GOP constituency. That constituency is hit a second time by a provision in the bill that allows insurers to charge older consumers more than young people, when compared to the ratio allowed under current law.
A 64-year-old at 175 percent of the poverty level who lives in a non-waiver state will pay eight times more in net premiums than under the current law.
Senate Republicans, led by the conference’s No. 3 Sen. John Thune (R-SD) have promised that they will rework the tax credits so the burden on older and lower-income people is less pronounced. But doing so may require shifting some of the tax benefit away from young and healthy people, who Republicans want to incentivize into buying insurance to make the risk pool less expensive.
Premiums in some places drop, but the costs are picked up elsewhere.
There was one number in the CBO report Republicans are likely to tout. The CBO predicted that about one-in-three Americans will live in states that seek waivers for “moderate” changes to the ACA’s insurer rules that would bring average premiums down by 20 percent by 2026 while maintaining relatively stable marketplace.
But those tweaks come with their downsides.
“Although premiums would decline, on average, in states that chose to narrow the scope of EHBs, some people enrolled in nongroup insurance would experience substantial increases in what they would spend on health care,” the CBO said, referring to the ACA’s 10 Essential Health Benefits, that states would be able to opt out of or rewrite under the GOP plan.
For years, Republicans have bashed Obamacare for how deductibles have increased under its implementation. Senators will now be contemplating a plan that will even further raise out-of-pocket costs.